 CONTACT US
CONTACT US
Dr Nico Coetzee
Dr Nico Coetzee
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Nico Coetzee
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Nico Coetzee
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Nico Coetzee
Dr Nico Coetzee
Dr Nico Coetzee
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Nico Coetzee
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Nico Coetzee
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Nico Coetzee
Dr Nico Coetzee
Dr Nico Coetzee
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Nico Coetzee
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Nico Coetzee
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Nico Coetzee
SPLEEN REMOVAL
How do I know if my spleen should be removed?
There are several reasons why a spleen might need to be removed, and the following list, though not all-
The most common reason is a condition called idiopathic (unknown cause) thrombocytopenia (low platelets) Purpura (ITP). Platelets are blood cells which aid is blood clotting. Hemolytic anemia (a condition that breaks down red blood cells) requires a spleen removal to prevent or decrease the need for transfusion. Also, hereditary (genetic) conditions that affect the shape of red blood cells, conditions known as Spherocytosis, sickle cell disease or thalassemia, may require Splenectomy. Often patients with cancers of the cells, which fight infection, known as lymphoma or certain types of leukemia, require spleen removal. When the spleen gets enlarged, it sometimes removes too many platelets from your blood and has to be removed. Sometimes the spleen is removed to diagnose or treat a tumor. Sometimes the blood supply to the spleen becomes blocked (infarct) or the artery abnormally expands (aneurysm) and the spleen needs to be removed.
How are these problems found?
An evaluation typically includes a complete blood count (cbc), a visual look at the blood cells placed on a glass slide called a ‘smear’, and often a bone marrow examination. Sometimes an ultrasound examination of your spleen, a computerized tomography (CT scan), magnetic resonance imaging (MRI) or nuclear scan is needed.
What are the advantages of laparoscopic Splenectomy?
Results may vary depending on your overall condition and health. Usual advantages are:
Less postoperative pain
Shorter hospital stay
Faster return to a regular, solid food diet
Quicker return to normal activities
Better cosmetic results
Am I a candidate for laparoscopic spleen removal?
Most patients can have a laparoscopic Splenectomy. Though the experience of the surgeon is the biggest factor in a successful outcome, the size of the spleen is the most important determinant in deciding whether the spleen can be removed laparoscopically. When the size of the spleen is extremely large, it is difficult to perform the laparoscopic
Technique. Sometimes, plugging the artery to the spleen right before surgery using special x-
What preparation is required?
After Doctor Coetzee reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
Preoperative preparation includes blood work, medical evaluation, chest x-
Immunization with a vaccine to help prevent bacterial infections after the spleen is removed should be given two weeks before surgery, if possible.
Blood transfusion and/or blood products such as platelets may be needed depending on your condition.
Dr Coetzee may request that you completely empty your colon and cleanse your intestines prior to surgery. You may be requested to drink clear liquids, only, for one or several days prior to surgery.
It is recommended that you shower the night before or morning of the operation.
After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon has told you are permissible to take with a sip of water the morning of surgery.
Drugs such as aspirin, blood thinners, anti-
Diet medication or st. John’s wort should not be used for the two weeks prior to surgery.
Quit smoking and arrange for any help you may need at home.
How is laparoscopic removal of the spleen done?
You will be placed under general anesthesia and be completely asleep. A cannula (hollow tube) is placed into the abdomen by your surgeon and your abdomen will be inflated with carbon dioxide gas to create a space to operate. A laparoscope (a tiny telescope connected to a video camera) is put through one of the cannulas which projects a video picture of the internal organs and spleen on a television monitor. Several cannulas are placed in different locations on your abdomen to allow your surgeon to place instruments inside your belly to work and remove your spleen. A search for accessory (additional) spleens and then removal of these extra spleens will be done since 15% of people have small, extra spleens. After the spleen is cut from all that it is connected to, it is placed inside a special bag. The bag with the spleen inside is pulled up into one of the small, but largest incisions on your abdomen. The spleen is broken up into small pieces (morcelated) within the special bag and completely removed.
What happens if the operation cannot be performed or completed by the laparoscopic method?
In a small number of patients the laparoscopic method cannot be performed. Factors that may increase the possibility of choosing or converting to the “open” procedure may include obesity, a history of prior abdominal surgery causing dense scar tissue, inability to visualize organs or bleeding problems during the operation.
The decision to perform the open procedure is a judgment decision made by Doctor Botha either before or during the actual operation. When Doctor Coetzee feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.
What can I expect after surgery?
After surgery you will be given intravenous fluids (iv’s) in your arm. You may have a stomach tube coming up out your nose to prevent vomiting or stomach bleeding because your stomach can fill up with stomach juices and not empty properly after this surgery. Not every surgeon uses this tube. You will be given pain medication to relieve the discomfort you may experience from the small incisions. You will need to let your nurse and surgeon know what your pain medication needs are since everyone has a different pain threshold.
As soon as you can resume oral intake, urinate, and care for your basic needs, you will typically be able to go home. Your surgeon will tell you when it is safe to go home.
Typically, once you have gone home, you may do the following, but each situation differs and “at home” activities should be discussed with Doctor Coetzee.
Activity: you can walk and go up stairs. You can shower, but most surgeons prefer that you do not soak in a tub for at least a week or more after surgery. When you feel stronger ask your surgeon about more strenuous activities.
Driving: ask your surgeon. Most people can resume driving 5 to 7 days after surgery. You should not be taking pain medication when you drive.
Diet: unless you have special dietary needs, such as diabetes, you can eat a normal diet at home.
Bowel function: it is common to get constipated after surgery, especially when you are taking pain medication. It is important to drink plenty of water and take in enough fiber in your diet. Your surgeon may advise you about means to help your bowel function postoperatively. Ask or call your surgeon before taking a cathartic.
What complications can occur?
Complications following laparoscopic Splenectomy are infrequent, but you should consult your doctor regarding possible complications based on your specific case. Possible complications may include cannula site infections, pneumonia, internal bleeding or infection inside the abdomen at the site where the spleen used to be, although these complications are infrequent. The pancreas can become inflamed (pancreatitis). Problems that can occur a few months to years later are hernias at the cannula sites or overwhelming infection throughout the entire body. This complication is also infrequent. Infection that occurs after Splenectomy is called Opsi.
Post-
When to call your doctor?
Be sure to call your physician or Doctor Coetzee if you develop any of the following:
- Persistent fever over 39°C
- Bleeding
- Increasing abdominal swelling
- Pain that is not relieved by your medications
- Persistent nausea or vomiting
- Chills
- Persistent cough or shortness of breath
- Purulent drainage (pus) from any incision
- Redness surrounding any of your incisions that is worsening or getting bigger
- You are unable to eat or drink liquids
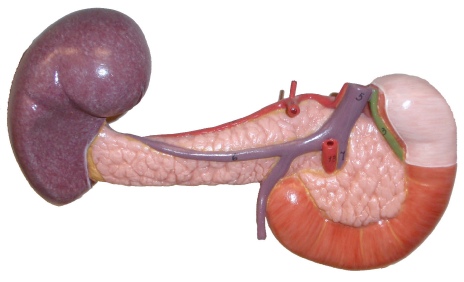
What is the spleen?
The spleen is a blood filled organ located in the upper left abdominal cavity. It is a storage organ for red blood cells and contains many specialized white blood cells called “macrophages” (disease fighting cells) which act to filter blood. The spleen is part of the immune system and also removes old and damaged blood particles from your system. The spleen helps the body identify and kill bacteria. The spleen can affect the platelet count, the red blood cell count and even the white blood count.