 CONTACT US
CONTACT US
Dr Nico Coetzee
Dr Nico Coetzee
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Nico Coetzee
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Nico Coetzee
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Nico Coetzee
Dr Nico Coetzee
Dr Nico Coetzee
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Nico Coetzee
Dr Coetzee specializes in Laparoscopic and Open surgery including certain areas of Surgical Oncology
Dr Nico Coetzee
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Coetzee joined the Medi Clinic group at Somerset West in 2009..Previously active and involved in the evolution of Laparoscopic Surgery as a participant and as an educator at Tygerberg Hospital in the Western Cape.
Dr Nico Coetzee
DIAGNOSTIC LAPROSCOPY
Diagnostic laparoscopy
Patients may be referred to surgeons because of an undiagnosed abdominal problem. If Doctor Coetzee has recommended a diagnostic laparoscopy, this page will:
Help you understand what laparoscopy is,
Describe how laparoscopy helps to find out what the problem is,
Explain what complications can occur with the procedure.
What is diagnostic laparoscopy?
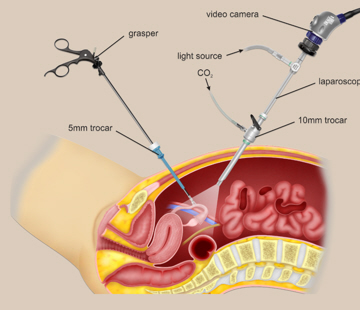
A laparoscope is a telescope designed for medical use. It is connected to a high intensity light and a high-
The laparoscope is put into the abdominal cavity through a hollow tube and the image of the inside of your abdomen is seen on the television screen. In most cases, this procedure (operation) will be able to diagnose or help discover what the abdominal problem is.
Why is diagnostic laparoscopy performed?
1. Abdominal pain.
Laparoscopy has a role in the diagnosis of both acute and chronic abdominal pain. There are many causes of abdominal pain. Some of these causes include appendicitis, adhesions or intra-
.

2. Abdominal mass.
A patient may have a lump (mass or tumor), which can be felt by the doctor, the patient, or seen on an x-
3. Ascites.
The presence of fluid in the abdominal cavity is called ascites. Sometimes the cause of this fluid accumulation cannot be found without looking into the abdominal cavity, which can often be accomplished with laparoscopy.
4. Liver disease.
Non-
5. “Second look” procedure or cancer staging.
Doctor Coetzee may need information regarding the status of a previously treated disease, such as cancer. This may occur after treatment with some forms of chemotherapy or before more chemotherapy is started. Also, information may be provided by diagnostic laparoscopy before planning a formal exploration of the abdomen, chemotherapy or radiation therapy.
6. Other.
There are other reasons to undergo a diagnostic laparoscopy, which cannot all be listed here. This should be reviewed and discussed with your surgeon.
What tests are necessary before laparoscopy?
Ultrasound may be ordered by your doctor as a non-
CT scan is an x-
MRI (magnetic resonance imaging) uses magnets, x-
Routine blood test analysis, urinalysis, and possible chest x-
What type of anesthesia is used?
Diagnostic laparoscopy is performed either under local anesthesia with sedation or with general anesthesia. With your help, your surgeon and an anesthesiologist will decide on a method of anesthesia to perform safe and successful surgery.
Local anesthesia can be injected into the skin of the abdominal wall to completely numb the area and allow safe placement of a laparoscope. Most patients feel a short-
General anesthesia is given to those patients who are not candidates for “twilight” sleep or who want to be completely asleep. General anesthesia may be preferable in patients who are young, who cannot lie still on the operating table, or have a medical condition that is safer to perform in this manner. Some patients end up having a general anesthesia even though they prefer local anesthesia with sedation, as the appropriate anesthesia for laparoscopy differs from patient to patient.
What preparation is required?
After Doctor Coetzee reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
It is acceptable to shower the night before or morning of the operation.
Most diagnostic laparoscopy procedures are performed as an outpatient; meaning you will go home the same day the procedure was performed.
You should have nothing to eat or drink for six to eight hours before the procedure.
Standard blood, urine, or x-
It is acceptable to shower the night before or morning of the operation. Report to the hospital at the correct time, which is usually 1-
If you take medication on a daily basis, discuss this with your surgeon prior to surgery, as you may need to take some or all of the medication on the day of surgery with a sip of water. If you take aspirin, vitamin e, blood thinners or arthritis medication, discuss this with your surgeon so they can be stopped at the proper time before your surgery.
You will need to ask Doctor Coetzee or his office staff what specifically is required in preparation for your surgery.
You will most likely be sedated during the procedure and an arrangement to have someone drive you home afterward is imperative. Sedatives will affect your judgment and reflexes for the rest of the day. You should not drive or operate machinery until the next day.
What can be expected during diagnostic laparoscopy?
The surgery is performed under anesthesia (see above), so that the patient will not feel pain during the procedure.
A cannula (a narrow tube-
A laparoscope (a tiny telescope) connected to a special camera is inserted through the cannula. This gives the surgeon a magnified view of the patient’s internal organs on a television screen.
Other cannulas are inserted which allow your surgeon to see the internal organs and make a decision on the proper diagnosis or treatment
After the surgeon completes the operation; the small incisions are closed with absorbable sutures or with surgical tapes.
What should I expect after the operation?
Following the operation, you will be transferred to the recovery room, where you will be monitored carefully until all the sedatives and anesthetics have worn off. Even though you may feel fully awake, the effects of any anesthetic may persist for several hours. Once you are able to walk and get out of bed unassisted, you may be discharged. Because the effects of anesthesia can linger for many hours, it is necessary to have someone accompany you to the office or hospital and drive you home after the procedure.
You can expect some soreness around any incision site; this is normal. Your pain should improve daily even though you may need to take a pain reliever. Your surgeon will instruct you on the use of pain relievers and may give you a prescription for pain medication. Most patients are able to shower the day after surgery and begin all normal activities within a week. Your surgeon can answer any specific restrictions that apply to you. You should call and schedule a follow-
What complications can occur?
Any procedure may have complications associated with it. The most frequent complications of any operation are bleeding and infection. There is a small risk of other complications that include, but are not limited to, injury to the abdominal organs, intestines, urinary bladder or blood vessels. If you suffer with ascites, this ascites may leak from one of the operative sites, temporarily, before stopping. In a small number of patients the laparoscopic method cannot be performed. The decision to perform the open procedure is a judgment decision made by Doctor Botha either before or during the actual operation. When Doctor Coetzee feels that it is safest to convert the laparoscopic procedure to an open
One, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.
When to call your doctor?
Be sure to call your surgeon or physician if you develop any of the following:
- Fever above 39°C
- Drainage from or redness any of your incisions
- Continued nausea or vomiting
- Increasing abdominal swelling
- Bleeding
- Chills
- Persistent cough or shortness of breath
- Inability to urinate
- Pain not controlled by medication